60 year old female complaining of loose stools and vomiting
ERLA SAI SHASI REDDY
ROLL NO : 182
9th semester
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis .
60 year old female complaining of loose stools and vomiting since 3 days and no urine output since two days .
Following is a brief about the case,
(History as per date of admission).
CHIEF COMPLAINTS:
A 60 year old female, daily wage labourer came to the Medicine OPD with complaints of:
• Loose stools, vomiting since 3 days.
• No urine output since 2 days.
HISTORY OF PRESENT ILLNESS:
Patient is a daily wage labourer since 15 years.
Seven days ago she gave a history of mutton consumption.
4 days later, the patient came with complaints of
Loose stools 5 -6 episodes/ day, watery in consistency, non mucoid, non bloodstained, non foul smelling.
Vomiting 4-5 episodes, bilious, non projectile with food as content.
No urine output since 2 days.
No history of pain abdomen, fever, body aches, burning micturition, cough, cold and shortness of breath.
HISTORY OF PAST ILLNESS:
• There is no history of similar complaints in the past.
• She is not a known case of DM, HTN, ASTHMA,TB, EPILEPSY.
• No history of surgeries in the past.
PERSONAL HISTORY:
Appetite- normal
Diet -mixed
Sleep - disturbed
Bowel and bladder - increased bowel movements and no urine output
No addictions, no known allergies for food or drugs.
FAMILY HISTORY:
No similar complaints in the family.
No significant family history.
GENERAL EXAMINATION:
Consent of the patient taken.
The patient is conscious,coherent and cooperative; well oriented to time,place and person.
She is moderately built and nourished.
• Pallor- present
• Icterus - absent
• Clubbing - absent
• Cyanosis - absent
• Lymphadenopathy - absent
• Edema - absent
VITALS
Temp : 98.6 F
PR : 82 bpm
RR : 24 cpm.
BP : 140/80 mm Hg
Spo2 : 97 %@ RA
Grbs : 107 mg/dl
SYSTEMIC EXAMINATION:
ABDOMEN EXAMINATION
INSPECTION:
Shape – scaphoid
Flanks – free
Umbilicus –central in position , inverted.
All quadrants of abdomen are moving with respiration.
No dilated veins, hernial orifices, sinuses
No visible pulsations.
PALPATION:
No local rise of temperature and tenderness
All inspectory findings are confirmed.
Deep palpation- no organomegaly.
PERCUSSION:
There is no fluid thrill , shifting dullness.
Percussion of liver for liver span
Percussion of spleen- dull note
AUSCULTATION:
Bowel sounds are heard.
CARDIOVASCULAR SYSTEM
INSPECTION:
Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
Apical impulse and pulsations cannot be appreciated
PALPATION:
Apical impulse is felt on the left 5th intercoastal space 2cm away from the midline.
No parasternal heave, thrills felt.
PERCUSSION:
Right and left heart borders percussed.
AUSCULTATION:
S1 and S2 heard , no added thrills and murmurs heard.
RESPIRATORY SYSTEM
INSPECTION:
Chest is bilaterally symmetrical
Trachea – midline in position.
Apical Impulse is not appreciated
Chest is moving normally with respiration.
No dilated veins, scars, sinuses.
PALPATION:
Trachea – midline in position.
Apical impulse is felt on the left 5th intercoastal space.
Chest is moving equally on respiration on both sides
Tactile Vocal fremitus - appreciated
PERCUSSION:
The following areas were percussed on either sides-
Supraclavicular
Infraclavicular
Mammary
Axillary
Infraaxillary
Suprascapular
Infrascapular
Upper/mid/lower interscapular were all RESONANT.
AUSCULTATION:
Normal vesicular breath sounds heard
No adventitious sounds heard.
CENTRAL NERVOUS SYSTEM EXAMINATION.
HIGHER MENTAL FUNCTIONS:
Patient is Conscious, well oriented to time, place and person.
All cranial nerves - intact
Motor system
Right. Left
BULK
Upper limbs. N. N
Lower limbs N. N
TONE
Upper limbs. N. N
Lower limbs. N. N
POWER
Upper limbs. 5/5. 5/5
Lower limbs 5/5. 5/5
Superficial reflexes and deep reflexes are present , normal
Gait is normal
No involuntary movements
Sensory system - all sensations ( pain, touch, temperature, position, vibration sense) are
well appreciated .
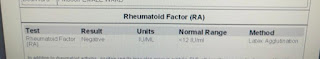
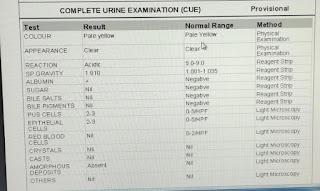
INVESTIGATIONS:
HB : 9.2
TLC: 13,100
PCV:28.3
PLT:2.78
N/L/M/E/B: 86/8/2/4/0
TLC: 13,100
PCV:28.3
PLT:2.78
N/L/M/E/B: 86/8/2/4/0
Urea : 112
Serum creatinine :5.4
Na :138
K : 3.3
Cl : 101
Serum creatinine :5.4
Na :138
K : 3.3
Cl : 101
PH : 7.08
Pco2:15.3
Po2: 113
Pco2:15.3
Po2: 113
Hco3: 7.1
Interpretation of ABG: high anion gap metabolic acidosis.
ECG:
PROVISIONAL DIAGNOSIS:
Acute GE with AKI.
TREATMENT:
1)IVF NS, RL, DNS @ 150 ml / hr
2)INJ. MONOCEF 1gm / i.v/ BD
3) INJ. METROGYL 100 ml /i.v/TID
2)INJ. MONOCEF 1gm / i.v/ BD
3) INJ. METROGYL 100 ml /i.v/TID
4) inj. LASIX 20 mg i.v BD
5) Syp.potchor 10ml in 1glass water BD
5) Syp.potchor 10ml in 1glass water BD
6) Plenty of oral fluids.